Executive Summary
In March 2014, as part of the RNAO-RPNAO Primary Care Toolkit development process, primary care colleagues in Ontario were invited to complete an online survey about the factors influencing the maximization of registered nurses (RN) and registered practical nurses’ (RPN) full scope of practice in primary care settings. Survey questions were informed by the literature and the expert opinion of those engaged in primary care work, and piloted with colleagues practicing in primary care settings, research associates, advisory team members, and the toolkit team. Free text option was embedded throughout the survey encouraging respondents to comment on the definition of full scope, factors contributing to role clarity, and suggestions for how a primary care toolkit on maximizing nurses’ full scope of practice would be most helpful to them. The survey was expected to take approximately five to seven minutes and answers were completely anonymous. Leading primary care associations were utilized to disseminate the survey to their members. Two reminder emails were sent. The survey was designed to inform the contents of the toolkit and the preliminary and final results were incorporated throughout the toolkit development process.
Analysis
Data were analyzed using SPSS 21, thematic analysis techniques, and weighted frequencies. Sub-group analyses by provider type and clinic type were also conducted. The tables included in this report represent the ranking of the weighted frequencies of the 12 factors as barriers and enablers from most critical to least critical barrier and from most important to least important enabler. The survey asked respondents to list their top three barriers from a choice of 12 variables. We applied a weighting representative of the 12 variables to the top three responses. We also analyzed the free text data using thematic analytic technique to determine what managers and directors wanted in the toolkit.
Demographics
199 participants completed the survey. Survey respondents included colleagues who held different positions at their respective organizations e.g. directors, managers, physicians, RNs, RPNs, and nurse practitioners (NP), and those from various clinic types e.g. Aboriginal Health Access Centres (AHAC), Community Health Centres (CHC), Family Health Teams (FHT) and Nurse Practitioner Led Clinics (NPLC).
Main findings
The findings indicate that most respondents did not think nurses (NP, RN, RPN) at their respective organizations practiced to full scope. Specifically, the majority of survey respondents did not think RNs and RPNs practised to full scope. There was also strong consensus that a lack of role clarity existed between all categories of nurses (RN, RPN, NP), and in particular, between RNs and RPNs.
Table 1: Ranking of the most critical barriers and most important enablers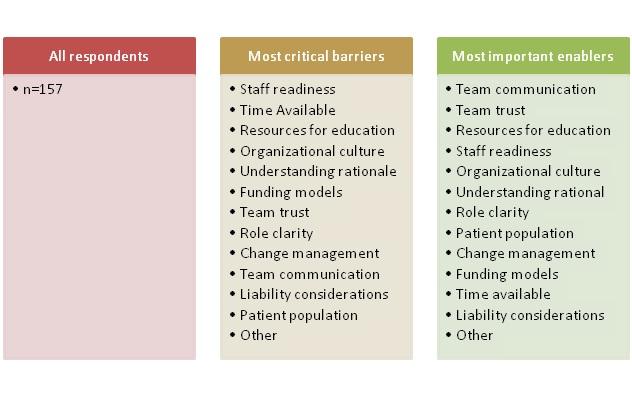
The table below represents the findings from the sub group analysis by clinic type. ’Staff readiness’ was viewed as the most critical barrier at two clinic types (CHC and ‘other’), whereas, ‘team communication’ was viewed as the most important enabler across almost all the clinic types (with the exception of AHAC).
Table 2: Subgroup analysis of the most critical barriers and most important enablers by clinic type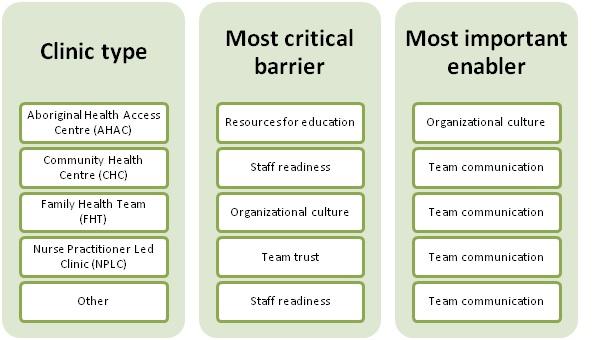
The table below represents the findings from the sub group analysis by provider type. Interestingly, RNs and RPNs thought that ‘understanding rationale’ for full scope was the most critical barrier which may have important implications for clinics and providers. ‘Team communication’ was reported as the most important enabler among almost all provider groups (with the exception of RNs, who identified team trust as most important).
Table 3: Subgroup analysis of the most critical barriers and most important enablers by provider type
Overall, the most critical barriers were ‘staff readiness’, ‘time available’, and ‘resources for education’ (see Table 1). However, sub group analyses by clinic type and job title yielded slightly different results which varied by clinic and provider type. For example, although ‘staff readiness’ was considered the most critical barrier overall, sub group analyses showed that it was only considered the most critical barrier at two clinic type models (CHCs and ‘other’) and considered the third most critical barrier at FHTs. With respect to provider types, this factor was consistently ranked in the top five among the list of barriers but never ranked as the most critical barrier.
Secondly, although ‘time available’ was considered the second most critical barrier overall, sub group analyses showed that it consistently ranked in the top five among the list of barriers by clinic type (excluding FHTs, where it ranked 11th), and by provider type (excluding the RPN job type group, where it was ranked 8th).
Finally, although ‘resources for education’ was identified as the third most critical barrier overall, sub group analyses showed that this factor was an important barrier among three clinic type models (AHACs, CHCs, and NPLCs), thus ranking in the top five among the list of barriers. Otherwise, ‘resources for education’ ranked in the top four list of barriers among all provider types (except for the RN group where it ranked 7th).
In addition, we learned that survey respondents wanted a toolkit that focused on the following:
- How to promote role clarity
- How to initiate conversations with staff members
- Information on change management
- Information about educational resources
- How to build trust
Thus, survey results were used to inform the development of some contents of the toolkit and identify the priority areas for which the toolkit should focus on.
Conclusion
The results of the survey make it clear that RNs and RPNs are not practising to their full scope in primary care settings. Further, there is a need for clinics to start examining ways to address barriers so that nurses’ full scope of practice utilization can be maximized in primary care settings. Finally, these results also tell us that there is a need for this toolkit to focus on clearly defining and distinguishing both RN and RPN roles and responsibilities in primary care settings, and between these roles when applicable.


