Figure 1: Percentage of Respondents (by Job Title) n=199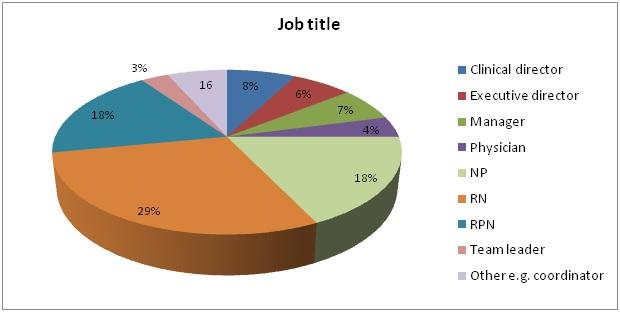
Survey respondents included those who held various job titles within primary care settings. Although there was most representation from RNs (29%), there was comparable representation from RPNs (18%) and NPs (18%). Directors, managers, physicians, team leaders, and ‘other’ were subsequently grouped into one category labelled, ‘other’ (below).
Figure 2: Percentage of Respondents (by Grouped Job Title) n=199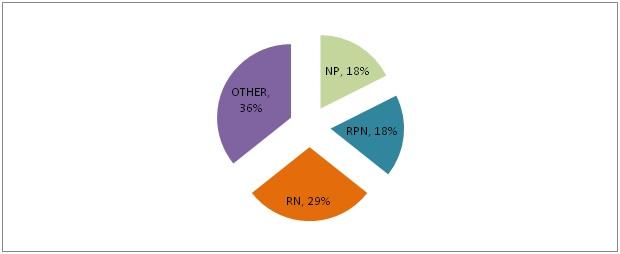
‘Other’ job title category included positions such as coordinator (3), telemedicine nurse (3), team lead (3), staff nurse (2), diabetes clinician/educator (2), outreach nurse, nurse specialist, and associate director.
Figure 3: Percentage of Respondents (by Clinic Type) n=199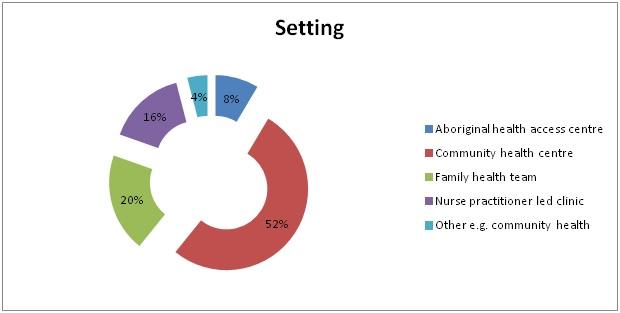
There was strong representation from community health centres (52%), followed by family health teams (20%) and nurse practitioner led clinics (16%). ‘Other’ clinic type category included clinics such as community mental health centre, patient enrolment models e.g. family health organizations (5), and ‘other’ (2). None of our survey respondents represented those practising from ‘solo practice’ settings.
Figure 4: Percentage of Respondents (by Region) n=199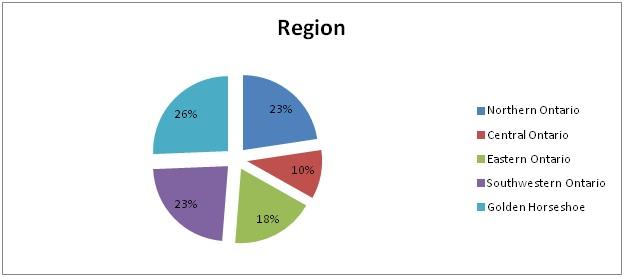
There was similar representation from all regions in Ontario except for central Ontario which included jurisdictions such as Peterborough, Belleville, and Orillia.
Meaning of maximizing nurses’ full scope of practice
Responses mainly centred around the notion of using all of a nurses’ skills (and knowledge) and practising within the limits of CNO and their respective organizations e.g. medical directives.
Full scope
Overall, 62.3% of survey respondents did not think the different categories of nurses worked to full scope while 37.7% thought that they did work to full scope (graphs not presented). A large majority of respondents identified NPs as working to full scope (45.2%) followed by RPNs (14.6%) and RNs (10.1%). The table below represents the sub group analysis of data by job title on whether each provider group type thought that nurses were working to full scope.
Figure 5: Are ALL nurses working to full scope in your setting (by Job Title) n=197 (2 responses missing)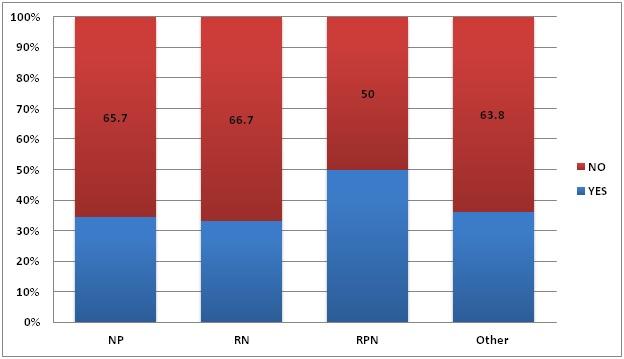
There was overwhelming consensus that all categories of nurses (RN, RPN, and NPs) were not working to full scope. However, respondents were equally divided on the question on whether they thought RPNs were working to full scope (50% yes, 50% no).
Sub group analysis
Please see below for a sub group analysis by job category (RN, RPN, NP, and other) and how each group responded to the question of whether they thought that RNs, RPNs, and NPs were working to full scope respectively. For the next graphs, we considered two questions as interlinked.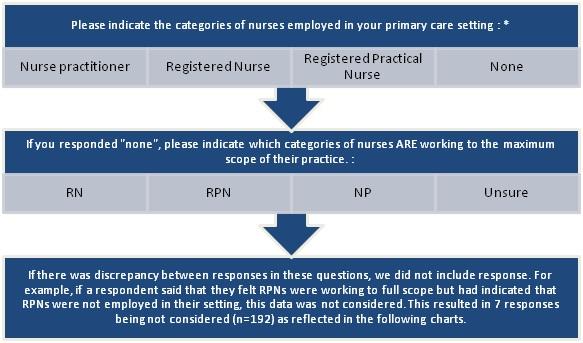
Sub group analysis: Job title
- Are RNs in your setting working to full scope? - Survey respondents overwhelmingly believed that RNs were not working to full scope at their respective organizations. Among provider groups, those grouped in the ‘other’ job title category least believed that RNs were not working to full scope (80.9%) whereas NPs most strongly believed that RNs were not working to full scope (97.1%).
- Are RPNs in your setting working to full scope? - Survey respondents overwhelmingly believed that RPNs were not working to full scope at their respective organizations. Among provider groups, RNs least strongly believed that RPNs were not working to full scope (79.6%) whereas NPs mostly strongly believed that RPNs were not working to full scope (94.3%).
- Are NPs in your setting working to full scope? - There were mixed results among survey respondents on the question of whether NPs were working to full scope. While 48.6% of NPs themselves said that they were not, others more strongly believed that they were not (52.9% to 78.8%) particularly the RPN group.
Sub group analysis: Clinic type
- Figure 9: Are ALL nurses working to full scope in your setting (by clinic type) n=197 - Of the 199 responses, 197 survey respondents were eligible for analysis. Participants from AHACs, CHCs, FHTs, and ‘other’ clinic types more strongly believed that nurses were not working to full scope at their respective settings, whereas participants from NPLCs believed that more nurses were working to full scope than were not working to full scope.
- Figure 10: Are RNs in your setting working to full scope (by clinic type) n=192 - Of the 199 survey respondents, 192 respondents were eligible. There was stronger consensus among clinic types that RNs were not working to full scope than were working to full scope. While on the low end were those grouped in the ‘other’ clinic types (75%), a high percentage of FHTs (97.4%) and NPLCs (93.5%) did not think that RNs were working to full scope.
- Figure 11: Are RPNs in your setting working to full scope (by clinic type) n=192 - Of the 199 survey respondents, 192 respondents were eligible. There was stronger consensus among clinic types that RPNs were not working to full scope than were working to full scope. While on the low end were those grouped in CHCs (47.5%), a higher percentage of FHTs (66.7%) and ‘other’ clinic types (66.7%) did not think that RPNs were working to full scope.
- Figure 12: NPs in your setting working to full scope (by clinic type) n=192 - Of the 199 survey respondents, 192 respondents were eligible for analysis. Except for CHCs (47.5%), sub group analysis revealed that all clinic types thought that more NPs were not working to full scope than were working to full scope.
Role clarity
Overall, 70.4% of survey respondents did not think there was role clarity between the different categories of nurses while 28.6% thought that there was role clarity between the different categories of nurses (graphs not presented). Respondents thought that having clear role descriptions and supportive organizational policies were important in addressing the lack of role clarity issue. More specifically, respondents thought that clearly distinguishing between RN and RPN roles was important. They also described the importance of educating team members about nurses’ roles and responsibilities as an important enabler.
Figure 13: Is there role clarity in your setting (by job title) n=197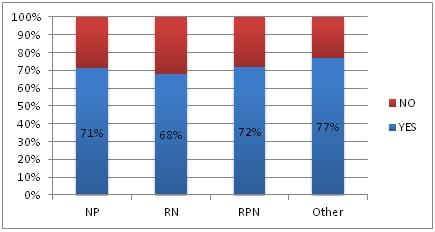
Of the 199 survey respondents, 197 responses were eligible for analysis. When grouped by job title, the majority of survey respondents believed that there was role clarity between the different categories of nurses.
Figure 14: Is there role clarity in your setting (by clinic type) n=197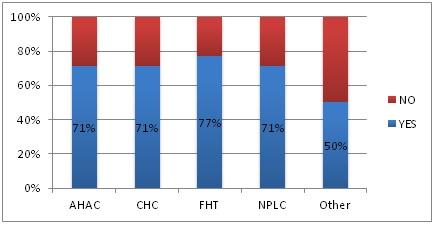
Similarly, when grouped by clinic type, the majority of clinic types felt that there was role clarity between the different categories of nurses. The exception was those clinics grouped in the ‘other’ category, of which only 50% felt that there was role clarity between the different categories of nurses.
Ranking of 12 factors as barriers and enablers
The following table presents the weighted frequencies of the 12 factors as barriers and enablers, as per the survey results. The survey asked respondents to list their top 3 top three barriers from a choice of 12 variables. To get these following tables, we applied a weighting representative of the 12 variables to the top 3 responses. The next table provides an overall representation of the barriers/enablers based on all respondents. N=157 as this question was optional.
Table 4: Most critical barriers and most important enablers to full scope of practice utilization for RNs and RPNs (by all respondents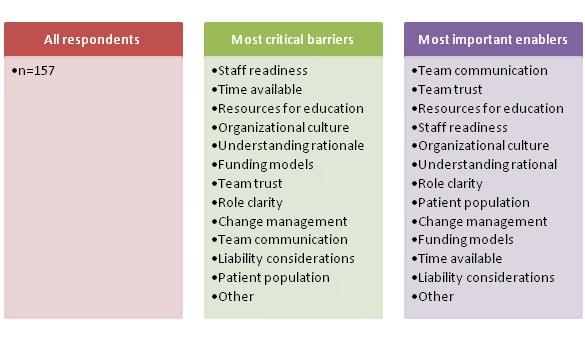
The barriers that received the fewest votes in general were patient population and liability. When we asked survey respondents to comment on how a toolkit would be helpful in overcoming their identified barriers, they said that it was important for team members to understand why full scope was needed and that clear processes for how organizations can achieve the goal of maximizing nurses’ full scope of practice in their setting would be helpful. In addition, survey respondents thought that an educational source that will increase role clarity, identify training/educational resources and opportunities for staff, and discuss the benefits of nurses practicing to full scope would be useful.
The most important enablers were communication, trust, and resources for education. The enablers that received the fewest votes in general were liability and time to work on this. Survey respondents largely felt that understanding of what full scope is and what the reasons and potential benefits are and knowing what resources are available to enhance nurses’ knowledge and skills, would lead to openness, trust, confidence, and eventually readiness. They felt that role clarity was extremely important, and should be highlighted, as well as steps for change management. When respondents were asked what other factors we should consider in developing this toolkit, their responses ranged from setting a minimum wage standard and hiring full time staff to providing examples of what a nurse working to full scope would look like.
Ranking of the 12 factors as barriers and enablers: Job title
Ranking of 12 factors as barriers and enablers: Clinic type


